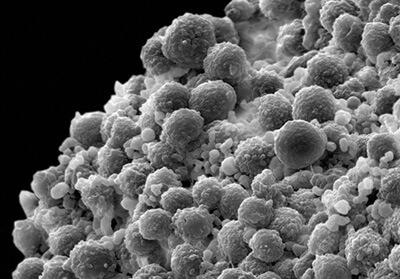
A scanning electron micrograph depicts a clump of prostate cancer cells. (Credit: Cell Image Library)
SAN DIEGO, Calif. — Your genes are a great way to screen for prostate cancer, suggests new research from the University of California (UC), San Diego. Their genetic test involved screening for 290 genetic variants and could provide doctors an extra tool for estimating a person’s risk for this deadly disease.
Second to skin cancer, prostate cancer is the most common cancer for men. According to the American Cancer Society, 268,490 cases are diagnosed each year, and 34,500 deaths. For a man living in the U.S., the chances of having future prostate cancer are 11% with a death risk of 2.5%.
“Men at highest risk of metastatic or fatal prostate cancer are potentially the most likely to benefit from screening or early detection,” says Meghana S. Pagadala, PhD, a medical and graduate student in the Medical Scientist Training Program at the UC San Diego School of Medicine and lead author of the study, in a press release.
Prostate cancer is often screened using the prostate-specific antigen (PSA) test. Doctor measures blood levels of a specific protein. The higher one's levels of the protein in their blood, the greater their chance of having prostate cancer and vice versa.
However, the PSA test is not a perfect screening tool and can cause false positives and negatives because of other influencing variables affecting PSA levels. What’s more, it’s unrealistic that every single person would come in for a screening with the potential of having to come back for unnecessary biopsies or treatment for low-grade cancer. It’s recommended for doctors to seek out additional tools such as an MRI before the biopsy.
“Current guidelines recommend doctors discuss the advantages and disadvantages of screening with their patients. The guidelines recommend stronger consideration of screening for men with highest risk, but it is not simple for primary care doctors to estimate a given patient’s risk of dying from prostate cancer. A comprehensive, objective assessment of each patient’s risk could make this much easier for doctors and patients,” explains senior study author Tyler M. Seibert, MD, PhD, an assistant professor in the departments of Radiation Medicine and Applied Sciences, Radiology and Bioengineering at UC San Diego School of Medicine.
The study authors conducted a genetic test that assessed for 290 genetic variants that are strongly associated with prostate cancer in almost 591,000 men in the Million Veteran Program. Most veterans were Black, which corresponds with a demographic often at high risk for prostate cancer. The median age of participants was 69.
“Current clinical guidelines for determining individualized risk assessment focus on race and ethnicity and family history,” says Seibert. “We’ve demonstrated in this study, based on a very large, diverse and longitudinal cohort, that a polygenic score adds considerably more information. Patients and their doctors can have a much better idea of which individuals are at highest risk of aggressive prostate cancer.”
The study is published in JNCI: Journal of the National Cancer Institute.