Cancer Treatment with Red Pills, Injections and Syringe. (© tashatuvango - stock.adobe.com)
SOLNA, Sweden — Immunotherapy has emerged as a powerful weapon in the fight against cancer. By unleashing the body's immune system to attack tumors, immunotherapy drugs like checkpoint inhibitors have led to dramatic recoveries for some patients with advanced cancers. However, these treatments don't work for everyone, and scientists are searching for ways to make them more effective.
Now, a team of researchers from the Karolinska Institutet may have found an ingenious new approach - using tiny biological delivery vehicles called extracellular vesicles to ferry immunotherapy drugs directly to tumors. Simply put, doctors may be able to put a message in a bottle that the body delivers directly to tumors.
These nano-sized vesicles, shed by cells as part of their normal functioning, have been engineered to display antibodies on their surface that guide them to specific targets. The result is an ultra-precise drug delivery system that accumulates in tumors while sparing healthy tissues. The study's results are published in the journal Nature Biomedical Engineering.
Extracellular vesicles are a diverse group of natural nanovesicles secreted by all cells. These nanovesicles range in size from 30 nm to 2,000 nm in diameter and can impact neighboring cells or cells at a distance. They contain lipids, proteins, and nucleic acid species from the source cell and uniquely convey these macromolecules through an advanced intercellular communication system. Importantly, extracellular vesicles benefit from the ability to cross biological barriers to reach distant organs, can be engineered to target specific atoms, and are loaded with a wide variety of therapeutic cargo molecules.
The researchers started with vesicles harvested from human cells grown in the lab. Using genetic engineering techniques, they adorned the vesicles with a special docking site — a fragment of a bacterial protein called protein A that binds tightly to antibodies.
“By attaching different antibodies to extracellular vesicles, we can target them to virtually any tissue and we can load them with other types of drugs as well,” says Oscar Wiklander and Doste Mamand, researchers in the Department of Laboratory Medicine at the Karolinska Institutet, in a media release. “Therefore, the treatment has the potential to be used against other diseases and cancer types.”
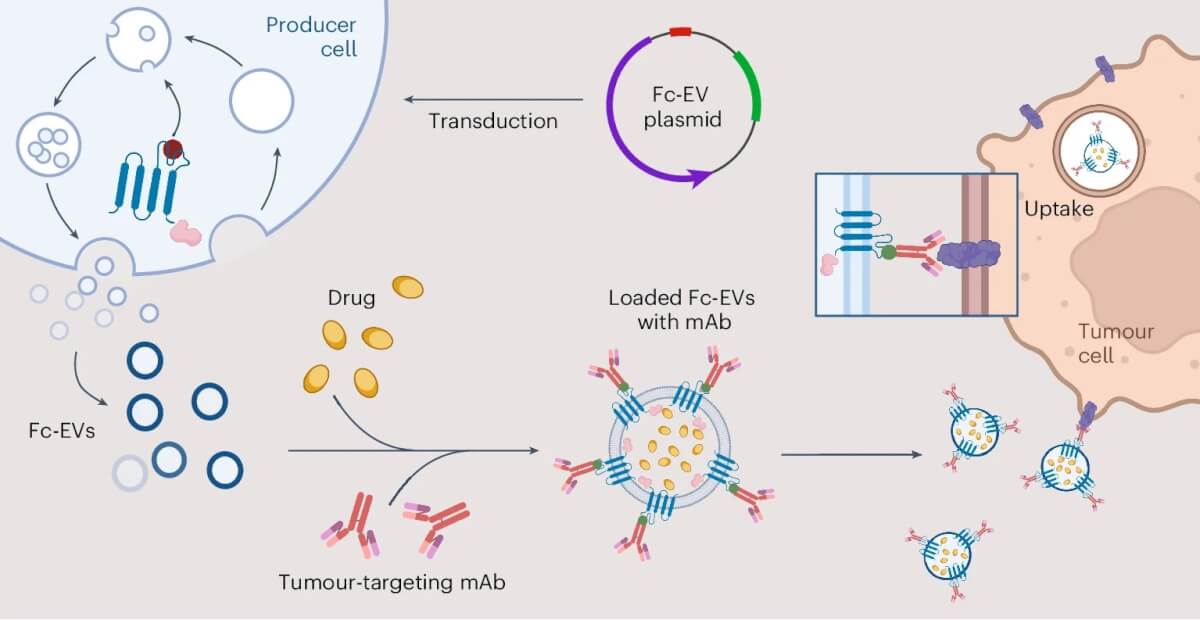
As an initial test, the team armed the vesicles with trastuzumab, an antibody drug used to treat breast cancers that make too much of a protein called HER2. They found that trastuzumab-coated vesicles were much better at homing to and penetrating HER2-positive breast cancer cells grown in lab dishes compared to naked vesicles. In mice bearing human breast tumors, a single injection of the antibody-coated vesicles led to significant accumulation in tumor tissue within just 30 minutes.
Next, the researchers tried vesicles coated with a different antibody called anti-PD-L1, which blocks a protein that cancer cells use to hide from immune attacks. Anti-PD-L1 drugs can be highly effective but often cause autoimmune side-effects by taking the brakes off the immune system throughout the whole body. By targeting the antibody's activity to tumors, the scientists hypothesized, they might increase efficacy and reduce toxicity.
When anti-PD-L1 vesicles were injected into mice with melanoma skin cancer, they accumulated in tumors at levels up to 180-fold higher than naked vesicles over three days. The vesicles also showed up in lymph nodes near the tumor, which serve as command centers for the immune response. Closer inspection revealed that the vesicles were gobbled up by tumor cells and immune cells expressing PD-L1.
Finally, the researchers packed the PD-L1-targeted vesicles with doxorubicin, a chemotherapy drug, creating a one-two punch of chemo-immunotherapy. Mice with melanoma treated with this combo had 100 percent survival at 20 days, compared to just 35 percent for untreated mice. Anti-PD-L1 or doxorubicin alone had little effect. Importantly, the treatment appeared safe, with no discernable kidney or liver toxicity.
The study demonstrates the potential of extracellular vesicles as a modular platform for delivering precision cancer therapies. By mixing and matching different antibodies and drug payloads, scientists could create bespoke treatments tailored to different cancer types.
Since extracellular vesicles are a natural product of human cells, they are less likely to trigger immune reactions or toxicity than synthetic nanoparticles made of plastics or metals that are currently used for drug delivery. Extracellular vesicles are also intrinsically better at penetrating tissues and being absorbed by cells.
While the technology still needs to be tested and optimized further before moving into human trials, the researchers are excited about the possibilities.
“Among other things, we want to investigate the possibility of delivering mRNA as an anticancer drug,” says the study’s last author, Samir EL Andaloussi, a professor in the Department of Laboratory Medicine at the Karolinska Institutet. “Ultimately, we hope this can lead to a new treatment platform that can improve treatment efficacy and reduce side effects in difficult-to-treat diseases, especially cancer.”
In an era of increasing interest in using the body's own resources to fight disease, extracellular vesicles are emerging as a new class of biological missiles that can be guided by molecular warheads to seek and destroy cancer cells. With further refinement, the tiny delivery trucks that cells use to send each other molecular mail could one day be repurposed to deliver bespoke cancer treatments on demand.
EdNews Editor-in-Chief Steve Fink contributed to this report.