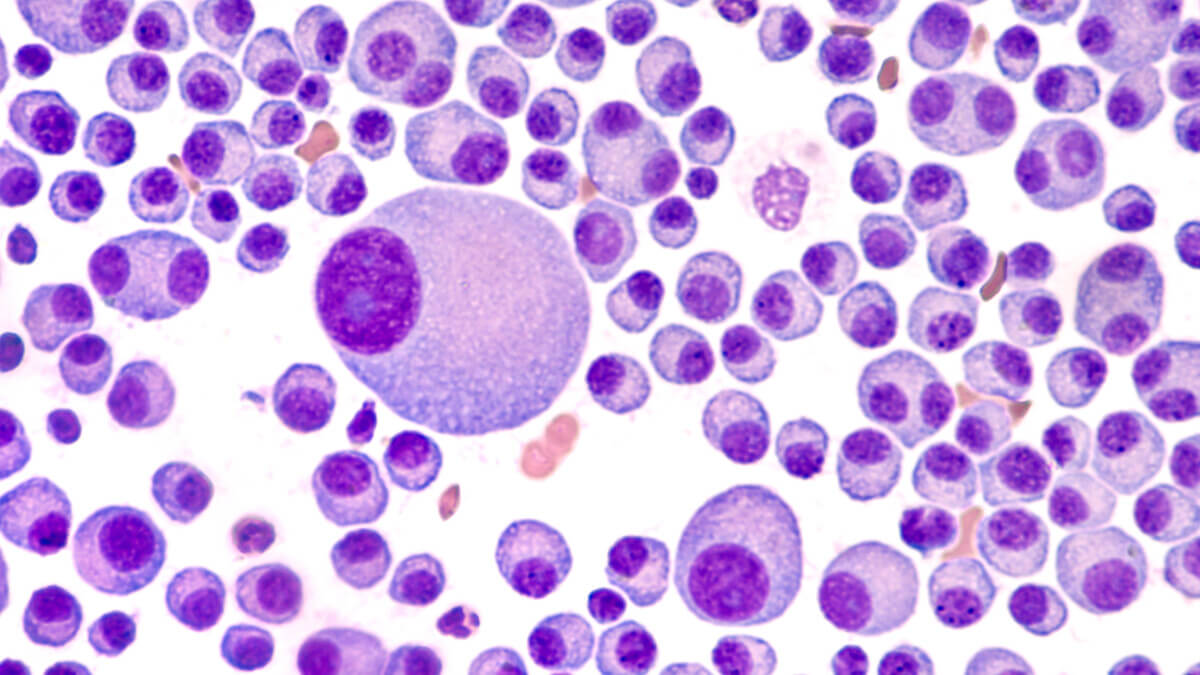
Bone marrow aspirate cytology of multiple myeloma, a type of bone marrow cancer of malignant plasma cells. (© David A Litman - stock.adobe.com)
SAN DIEGO, Calif. — For patients with multiple myeloma, a form of blood cancer, taking a single treatment is not an option. This is because the disease quickly develops a resistance to cancer drugs, forcing doctors to change course. A new study finds one of the main reasons myeloma adapts is because of its cancer stem cells, which keep renewing themselves. Researchers at University of California-San Diego School of Medicine and Ionis Pharmaceuticals say they may finally have a way to stop that process. Their new treatment literally wipes away all traces of the disease in experiments on mice.
Study authors say that if a cancer therapy doesn't completely destroy cancerous stem cells, the disease will keep coming back. In their experiments, researchers targeted IRF4, a gene which allows myeloma stem cells and tumors to multiply and survive. According to previous studies, the more IRF4 a cancer patient has, the worse their chances of survival are.
Designed to kill cancer
The new treatment uses an engineered piece of DNA (an antisense oligonucleotide) specifically designed to bind the genetic material coding of IRF4. This oligonucleotide, which Ionis calls ION251, causes the gene to degrade. Tests reveal that ION251 lowers the number of myeloma stem cells and increases survival rates among mice dealing with human myeloma.
The results are so promising a Phase I clinical trial is getting underway which hopes to prove the treatment's safety and effectiveness on human patients.
One challenge facing myeloma researchers is the fact that myeloma cells don’t grow well in laboratory settings. To overcome this, researchers transplant human myeloma cells directly into mice who lack an immune system. This keeps the animals from rejecting the new cells and essentially creates an “avatar” of a cancer patient.
The UCSD team tested ION251 on their own myeloma avatars during the study. Researchers gave 10 mice ION251, while another 10 mice went untreated to serve as a control group. Mice on ION251 received a daily dose of the drug for one week before switching to three doses per week for the rest of the experiment.
After two to six weeks of treatment, mice on ION25 had significantly fewer myeloma cells in their bodies. Between 70 and 100 percent of the treated mice survived. In comparison, none of the untreated mice lived through the whole study.
Already showing promise on human cells
In a separate phase of the study, researchers discovered that human cells treated with ION251 also saw positive results. The treatment destroyed myeloma stem cells while sparing healthy blood cells.
“The results of these preclinical studies were so striking that half the microscopy images we took to compare bone marrow samples between treated and untreated mice kept coming back blank — in the treated mice, we couldn’t find any myeloma cells left for us to study,” co-senior author Leslie Crews from UCSD says in a university release. “It makes the science more difficult, but it gives me hope for patients.”
In addition to its significant cancer-fighting results, the treatment is also helping scientists understand the mechanisms which work to inhibit IRF4. The new information is clearing up how myeloma initially develops in patients.
“These proof-of-principle studies will enable rapid clinical development of anti-sense oligonucleotide-mediated IRF4 inhibition to prevent myeloma relapse driven by drug-resistant cancer stem cells,” says co-senior author Catriona Jamieson.
“As scientists, we don’t usually have direct contact with patients, as a daily reminder of what our research could do, or why it’s important,” Crews adds. “But I’ve been working with a local support group for patients with multiple myeloma. They inspire me. They ask the most insightful questions, and it really makes it personal. I hope this work will eventually give them new potential treatments to prevent relapse, and ultimately get better.”
The study appears in the journal Cell Stem Cell.