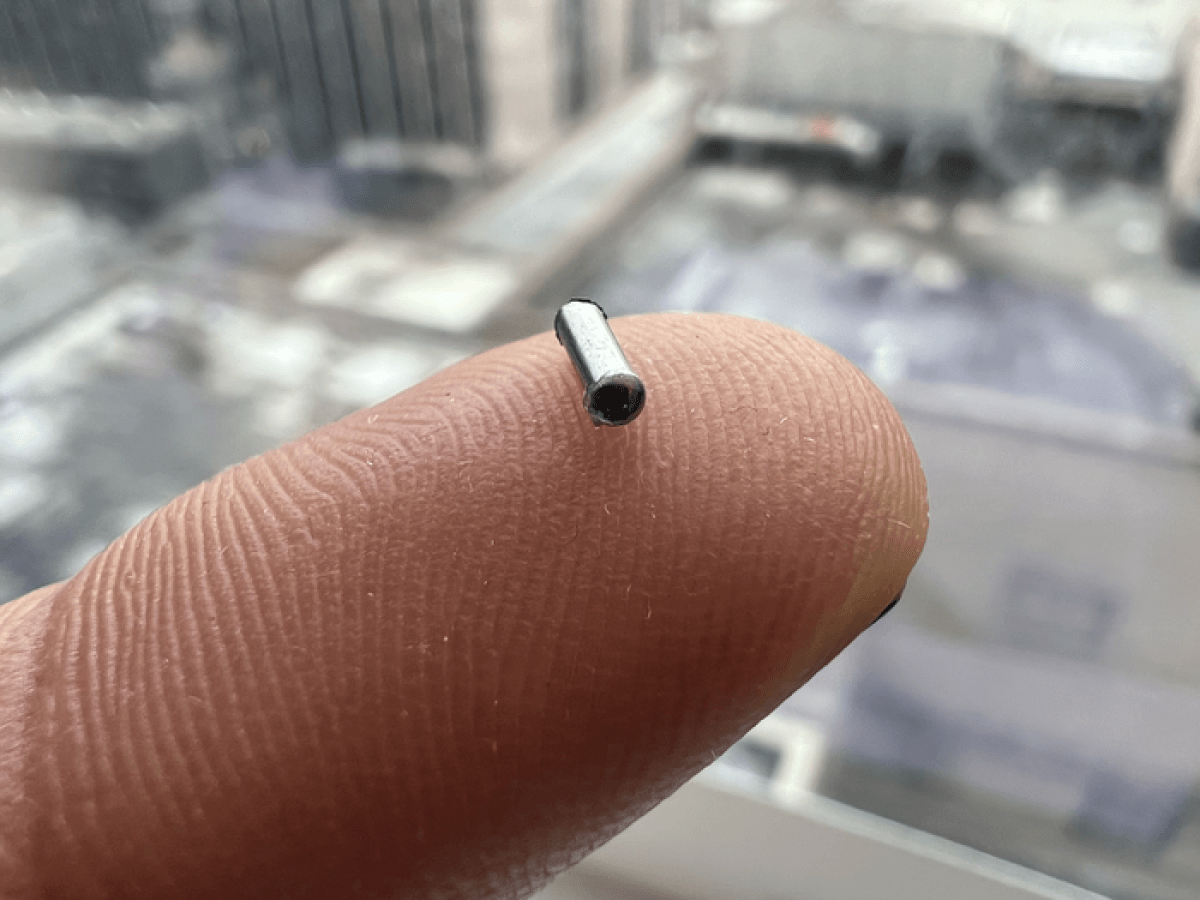
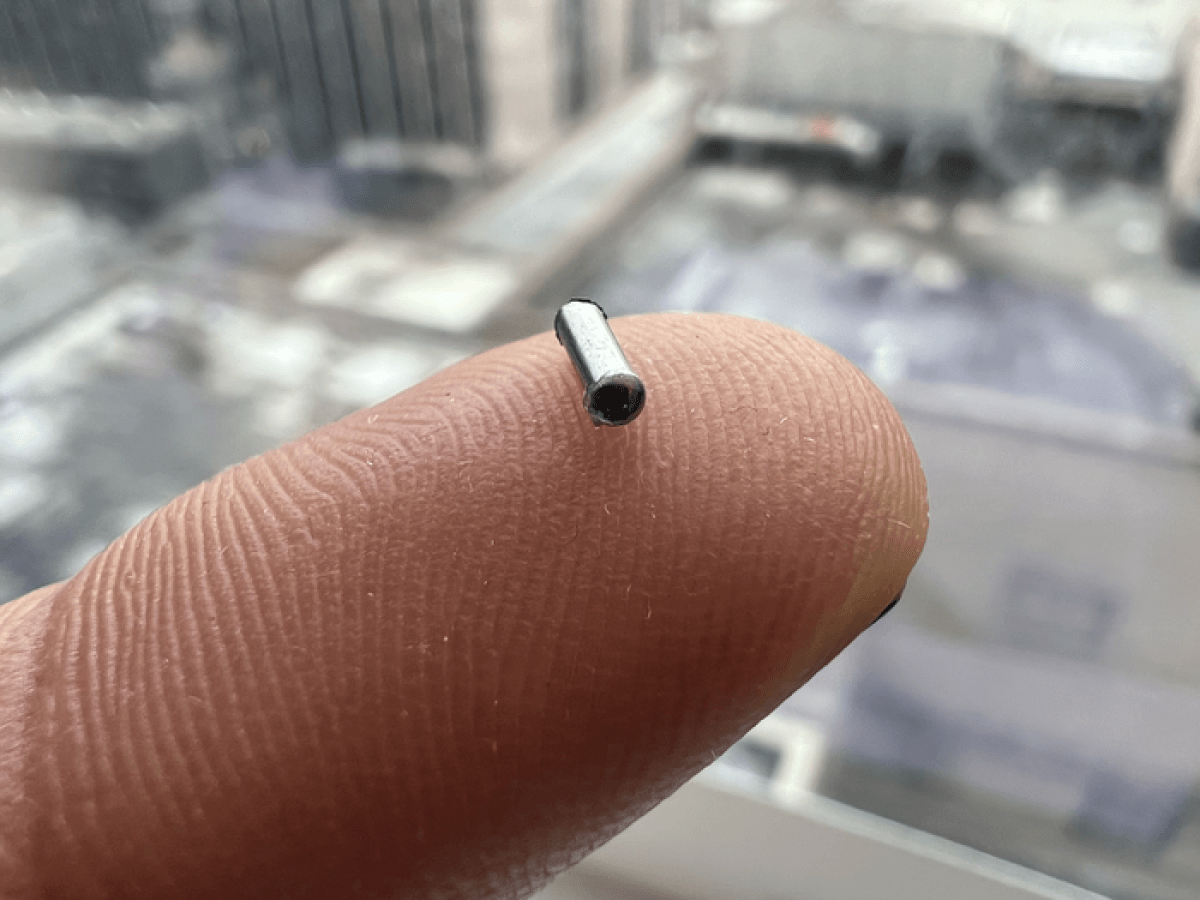
Houston Methodist Research Institute nanomedicine researchers used an implantable nanofluidic device smaller than a grain of rice to deliver immunotherapy directly into a pancreatic tumor. CREDIT: Houston Methodist
HOUSTON — Scientists at the Houston Methodist Research Institute have designed a potentially groundbreaking new device for treating pancreatic cancer, and it's smaller than a single grain of rice. Pancreatic cancer is one of the most aggressive forms of the disease and one of the hardest to treat, but this new implantable device is capable of delivering immunotherapy directly into tumors.
Study authors invented, developed, and tested an implantable nanofluidic device for delivering CD40 monoclonal antibodies (mAb), a promising immunotherapeutic agent, at a sustained low-dose via the nanofluidic drug-eluting seed (NDES). The end result, observed in murine models, was tumor reduction at a four-fold lower dosage than traditional systemic immunotherapy treatment. Simply put, the device needs less medicine to shrink cancerous tumors.
“One of the most exciting findings was that even though the NDES device was only inserted in one of two tumors in the same animal model, we noted shrinkage in the tumor without the device,” says Corrine Ying Xuan Chua, Ph.D., co-corresponding author and assistant professor of nanomedicine at Houston Methodist Academic Institute, in a media release. “This means that local treatment with immunotherapy was able to activate the immune response to target other tumors. In fact, one animal model remained tumor-free for the 100-days of continued observation.”
Doctors most often diagnose pancreatic cancer at advanced stages
By then, the cancer is much harder to treat. More specifically, roughly 85 percent of patients already have metastatic disease at diagnosis, meaning the cancer is spreading to other parts of the body.
Houston Methodist researchers are currently studying similar nanofluidic delivery technology on the International Space Station. Grattoni’s nanomedicine lab at Houston Methodist, meanwhile, is focusing on implantable nanofluidics-based platforms designed for controlled and long-term drug delivery and cell transplantation in order to treat various chronic diseases.
Immunotherapy holds particular promise when it comes to treating cancers that don't respond to typical treatments. However, since immunotherapy affects the entire body, it can also cause many side-effects that can sometimes be long-lasting, if not life-long. By using this new device to deliver treatment directly into the tumor, doctors can protect the rest of patients' bodies from exposure to toxic drugs. In turn, this will lead to fewer side-effects, consequently allowing cancer patients to enjoy an overall better quality of life.
“Our goal is to transform the way cancer is treated. We see this device as a viable approach to penetrating the pancreatic tumor in a minimally invasive and effective manner, allowing for a more focused therapy using less medication,” explains Alessandro Grattoni, Ph.D., co-corresponding author and chair of the Department of Nanomedicine at Houston Methodist Research Institute.
The device lasts longer than typical implants
The NDES device consists of a stainless-steel drug reservoir featuring nanochannels, which creates a membrane facilitating sustained diffusion when releasing the drug. While other medical tech companies do offer intratumoral drug-eluting implants for cancer therapeutics, those are typically in use for shorter durations. The study authors designed the nanofluidic device for long-term controlled and sustained release. This should help avoid the repeated systemic treatments that often leads to adverse side-effects.
Moving forward, scientists are conducting more lab research to help determine the effectiveness and safety of this delivery technology. All in all, researchers say they would like to see this become a viable option for cancer patients in the next five years or so.
The study authors describe the implant in the journal Advanced Science.