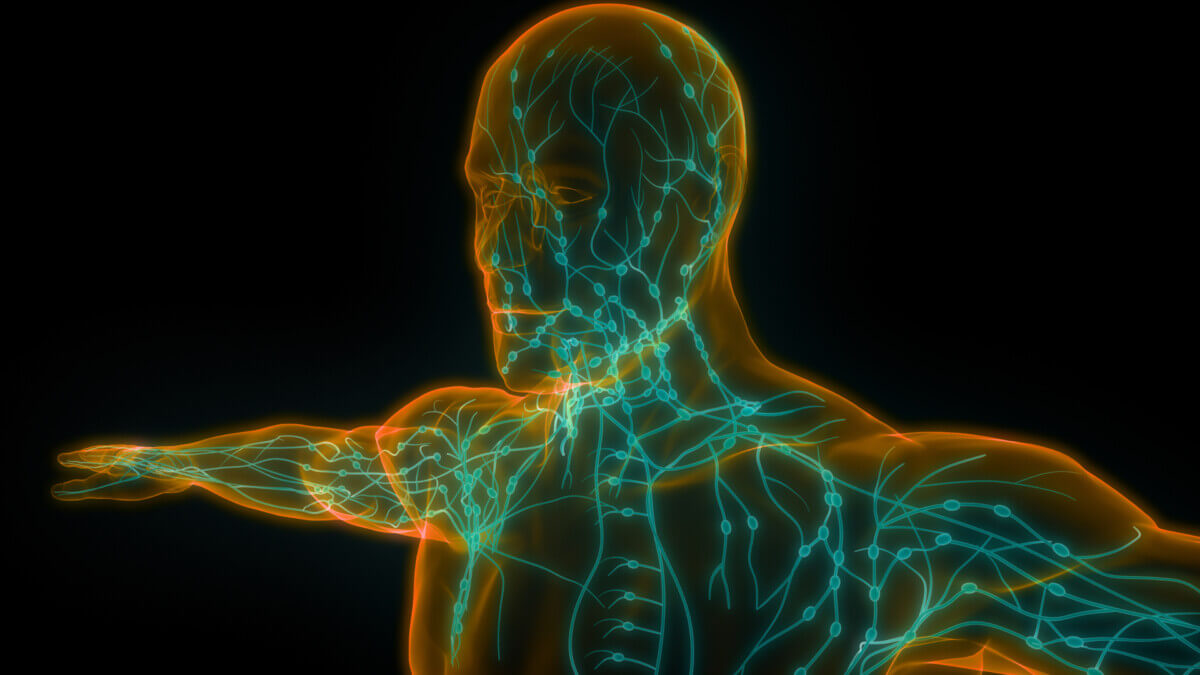
(Credit: Magic mine/Shutterstock)
BALTIMORE — Imagine a world where we could harness the power of our own immune system to fight cancer without the need for grueling chemotherapy or invasive surgeries. Researchers at Johns Hopkins University have taken a major step towards making this vision a reality with the development of an artificial lymph node (aLN) that can stimulate the body's natural cancer-fighting T cells directly inside the body. This groundbreaking technology has the potential to revolutionize cancer treatment and bring new hope to millions of patients worldwide.
How It Works:
The aLN is a tiny scaffold made of a jelly-like substance called hyaluronic acid, which is already found naturally in the body. The scientists load this scaffold with three key ingredients that are essential for activating cancer-fighting T cells:
- Fragments of the cancer proteins that the immune system needs to recognize (Signal 1)
- Molecules that provide co-stimulation to the T cells (Signal 2)
- A specially engineered version of a T cell-stimulating cytokine called IL-2 (Signal 3)
When this aLN scaffold is injected under the skin, it creates a specialized microenvironment that mimics a real lymph node. Naive T cells (the rookies of the immune system) are recruited to this artificial lymph node, where they receive the three signals they need to become activated cancer killers. Importantly, the IL-2 cytokine is tethered to the scaffold using an antibody, which makes the IL-2 signal persist longer and preferentially stimulate the cancer-fighting T cells over regulatory T cells that could hinder the anti-tumor response.
Putting Artificial Lymph Nodes To The Test
To test their aLN, which the team unveiled in the journal Advanced Materials, the researchers first optimized the stiffness and concentration of the three signals in the scaffold to maximize T cell stimulation.
Next, they tested the aLN's ability to stimulate rare cancer-specific T cells, both from model mice with genetically engineered T cells and from normal mice with natural T cell repertoires. Impressively, a single injection of the aLN particles loaded with cancer antigens could dramatically expand the population of cancer-fighting T cells over the course of seven to nine days - up to 11,000 times in some cases! The stimulated T cells were functional, too, able to kill cancer cells pulsed with their target antigen both in a dish and in living animals.
Critically, the efficacy of the aLN was enhanced when the host's natural immune system was intact. When the scientists peered inside the aLN over time, they found a dynamic influx of various immune cells, including dendritic cells, macrophages, and CD4 “helper” T cells that created a natural support system to further boost the cancer-fighting CD8 T cells.
The Results: Shrinking Tumors and Extending Survival
To see if their aLN-activated T cells could actually fight cancer, the scientists tested their approach in several mouse models of melanoma and colon cancer. When they injected naive T cells together with the aLN particles one week before implanting the tumors, the aLN treatment significantly delayed tumor growth and extended the animals' survival compared to untreated mice.
The aLN was even able to shrink existing tumors when given to mice with palpable tumors, especially when combined with a checkpoint inhibitor drug. This suggests the aLN could be a valuable addition to current cancer immunotherapies.
Limitations and Next Steps
While these initial results in mice are highly promising, the aLN still needs to be rigorously tested for safety and efficacy in humans. A potential limitation is that cancer patients often already have some pre-existing tumor-reactive T cells, and it's unclear if the aLN will be as effective at boosting these pre-activated cells compared to fully naive T cells. More studies are needed to optimize the aLN formulation for clinical translation.
Off-The-Shelf Cancer Immunotherapy?
Looking ahead, the aLN's modular and tunable design offers exciting opportunities to incorporate additional immune-stimulating drugs and tailor the platform for different cancer types. The scientists showed that the aLN could even activate human cancer-fighting T cells in a dish, a key first step toward clinical translation.
“We blended the disciplines of materials science and immunology to create a potential therapy that forms its own immunology community — a kind of living drug,” says Dr. Jonathan Schneck, a professor of pathology, medicine and oncology at the Johns Hopkins University School of Medicine. He is also the director of the Johns Hopkins Center for Translational Immunoengineering.
“An advantage to this approach over other cell-based therapies such as CAR-T is fewer manufacturing steps,” he adds.
If the aLN proves safe and effective in patients, it could potentially offer an “off-the-shelf” immunotherapy for cancer. Rather than having to isolate and engineer a patient's T cells in a lab - an expensive and time-consuming process - doctors could simply inject the aLN particles loaded with cancer antigens to activate the patient's own T cells inside their body. This could greatly expand access to cutting-edge cancer immunotherapies.
While there is still much work to be done, the artificial lymph node represents an exciting leap forward in our ability to manipulate the immune system to fight cancer. By bringing the power of immune engineering directly into patients' bodies, this new technology holds immense promise for expanding the scope and accessibility of cancer immunotherapy in the future.





I am a medical anthropologist and pioneer of applied medical anthropology, where I focus on the cultural causes of disease. Most cancer is caused by interfering with our body’s immune system. Perhaps that is why this study is trying to come up with artificial lymph nodes. But there is a flaw in the article above.
“Imagine a world where we could harness the power of our own immune system to fight cancer without the need for grueling chemotherapy or invasive surgeries.” I have great news! We already have this. Our immune system fights cancer all the time. Cancer cells develop constantly, and our immune system destroys them, if our culture and the things it makes us do to ourselves don’t get in the way.
Cancer, then, is really a problem of immune system dysfunction. When immunity fails, cancer develops unchallenged. This study is trying to make artificial lymph nodes, but people need to take better care of their own, natural lymph nodes and lymphatic system.
A big problem medicine is that it ignores a major cultural cause of immune dysfunction, which is tight clothing. This is especially true for breast cancer, given that breasts are typically constricted by tight bras in bra-using cultures. This impairs immune function by constricting and compressing the lymphatic vessels that protect the breasts from cancer cells developing. The material in bras also can leach toxic chemicals into the breast skin. These toxins concentrate in the breasts due to the lymphatic constriction from bras. Bras essentially cause fluid congestion in the breasts with associated toxification and reduced immune function. Many studies internationally show a link between bra usage and breast cancer incidence.
Studies done on rats do not model the impact of tight clothing on lymphatic function and, hence, on immune function. Medicine typically ignores the impact of clothing, perhaps because they rely on animal models. On the other hand, doctors are part of the culture which uses tight clothing, and many wear tight clothing themselves.
Immune function requires proper circulation above all else. Creating artificial lymph nodes will not help if there is poor circulation.
See my article Tight Clothing Affects Tumor Microenvironment. https://www.academia.edu/114117362/Tight_Clothing_Affects_Tumor_Microenvironment
“This is especially true for breast cancer, given that breasts are typically constricted by tight bras in bra-using cultures.”
I see what you are trying to do. lol